Imagine being able to receive precise and effective medical treatment without the need for extensive surgery or long recovery times. With interventional radiology, you can experience just that.
This groundbreaking field utilizes minimally invasive procedures to accurately diagnose and treat various conditions. From reducing the risk of complications to offering outpatient treatment options, the benefits of interventional radiology are vast.
However, like any medical intervention, there are also considerations to be aware of. In this article, we explore the pros and cons of interventional radiology, helping you make informed decisions about your healthcare.
Key Takeaways
- Minimally invasive procedures in interventional radiology offer numerous benefits such as reduced trauma to the body, lower risk of complications, shorter hospital stays, and quicker recovery times.
- Advancements in technology have led to increased accuracy and precision in interventional radiology procedures, allowing for precise targeting of affected areas and better outcomes for patients.
- Faster recovery time is another advantage of interventional radiology, thanks to small incisions, specialized tools, and minimal trauma to the body.
- Outpatient treatment in interventional radiology offers convenience, cost-effectiveness, and minimal disruptions to daily activities, allowing patients to return home the same day and resume their normal routines.
Increased Accuracy and Precision
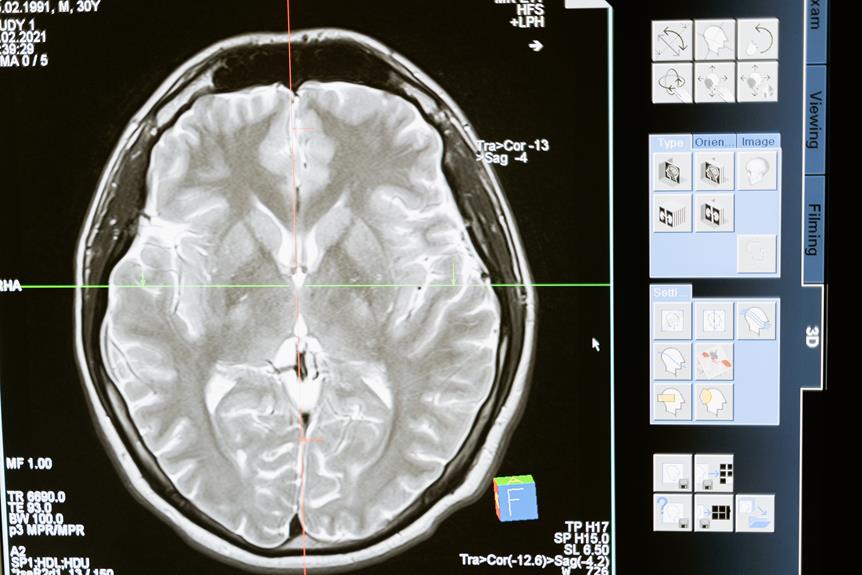
You should consider the benefits of increased accuracy and precision in interventional radiology. When it comes to medical procedures, accuracy and precision are of utmost importance. With advancements in technology, interventional radiology has made significant strides in improving accuracy and precision in various procedures.
One of the key benefits is the ability to precisely target specific areas within the body, minimizing damage to surrounding healthy tissues. This is particularly crucial in delicate procedures such as tumor ablation or angioplasty.
Increased accuracy and precision also lead to better outcomes for patients. By precisely locating and treating the affected area, interventional radiologists can ensure that the treatment is effective and that any potential risks are minimized. This can result in shorter recovery times, reduced complications, and improved patient satisfaction.
Another advantage is the ability to perform complex procedures with greater confidence. Advanced imaging techniques, such as fluoroscopy and CT scans, allow interventional radiologists to visualize the procedure in real-time. This enables them to make immediate adjustments and ensure that the intervention is performed with utmost accuracy.
Minimally Invasive Procedures
When it comes to minimally invasive procedures, you'll find a range of benefits. These non-surgical techniques offer improved patient recovery, as they cause less trauma to the body.
Additionally, they come with a lower risk of complications compared to more invasive methods.
Benefits of Non-Surgical Techniques
Using non-surgical techniques can provide significant benefits in terms of minimizing recovery time and reducing scarring. When you opt for non-surgical procedures, you can avoid the risks and complications associated with invasive surgeries.
These techniques, such as interventional radiology, offer a less invasive approach to treating various medical conditions. By using imaging guidance and specialized tools, interventional radiologists can perform a wide range of procedures without the need for open surgery. This means shorter hospital stays, less pain, and quicker recovery times for you.
Additionally, non-surgical techniques often result in minimal scarring or even no visible scars at all, improving your overall aesthetic outcome.
Improved Patient Recovery
Minimally invasive procedures often lead to improved patient recovery, allowing for quicker healing and reduced hospital stays. When you opt for a minimally invasive procedure, such as laparoscopy or arthroscopy, you can expect several benefits that contribute to your overall recovery.
Here are some advantages of minimally invasive procedures:
- Smaller incisions: With smaller incisions, you experience less pain and discomfort during the recovery process.
- Reduced risk of infection: Since the incisions are smaller, the risk of infection is significantly lowered, leading to a faster healing process.
In addition to these benefits, minimally invasive procedures also offer other advantages that contribute to a better patient recovery experience. By minimizing trauma to the body, these procedures result in less blood loss, reduced scarring, and shorter hospital stays.
Less Risk of Complications
You'll experience fewer complications with minimally invasive procedures, resulting in a smoother recovery process.
When it comes to medical interventions, complications can be a source of stress and anxiety. However, with minimally invasive procedures, the risk of complications is significantly reduced.
These procedures use small incisions and advanced technology to perform surgeries or treatments, minimizing damage to surrounding tissues and organs.
The benefits of this approach are numerous. Not only do you have a lower chance of developing infections or bleeding, but you also experience less pain and scarring.
Additionally, the recovery process is often faster, allowing you to get back to your normal activities sooner.
Minimally invasive procedures have revolutionized the medical field, providing safer and more efficient options for patients like you.
Reduced Risk of Complications
You can experience fewer complications with interventional radiology procedures. When it comes to medical treatments, complications are always a concern. However, with interventional radiology, the risk of complications is significantly reduced. Here's why:
- Minimally invasive: Interventional radiology procedures are performed using small incisions or catheters, minimizing the risk of infection and reducing the recovery time.
- Precise targeting: Through imaging guidance, interventional radiologists can accurately target the affected area, ensuring that the treatment is delivered exactly where it's needed. This precision minimizes the risk of damage to surrounding tissues.
These two factors play a crucial role in reducing complications and improving patient outcomes. By opting for interventional radiology procedures, you can have peace of mind knowing that the risks associated with traditional surgeries are significantly reduced. This approach not only leads to a smoother recovery but also allows for quicker return to normal activities.
Remember, when it comes to your health, it's essential to explore all available options. Interventional radiology offers a safer alternative to traditional surgeries, providing you with the opportunity to experience fewer complications and a faster recovery.
Talk to your healthcare provider to see if interventional radiology procedures are suitable for your specific condition.
Faster Recovery Time
With interventional radiology, you can experience fewer complications and a faster recovery time. This innovative medical field combines imaging technology with minimally invasive procedures to treat a wide range of conditions. Whether you're dealing with a vascular issue, cancer, or chronic pain, interventional radiology offers numerous benefits.
One of the major advantages of interventional radiology is its ability to provide a faster recovery time compared to traditional open surgeries. By utilizing small incisions and specialized tools, interventional radiologists can perform procedures with minimal trauma to the body. This means less pain, reduced scarring, and a quicker return to your normal activities.
To help you visualize the impact of interventional radiology on recovery time, here's a table comparing the average recovery period for common procedures:
| Procedure | Traditional Surgery | Interventional Radiology |
|---|---|---|
| Angioplasty | 1-2 weeks | 1-2 days |
| Tumor Ablation | 4-6 weeks | 1-2 days |
| Pain Management | Ongoing | Immediate relief |
| Embolization | 1-2 weeks | 1-2 days |
| Drainage Procedures | 2-4 weeks | 1-2 days |
As you can see, interventional radiology offers a significant reduction in recovery time across various procedures. This means less time spent in the hospital and more time enjoying life.
Potential for Outpatient Treatment
You'll be pleased to know that outpatient treatment offers several advantages.
Firstly, it provides the convenience of receiving medical care without the need for hospitalization, allowing you to return home the same day.
Additionally, outpatient care is often more cost-effective than inpatient care, which can help lower your healthcare costs.
Lastly, outpatient treatment is known for its faster recovery time, meaning you can resume your daily activities sooner.
Convenience of Outpatient Care
An article on The New York Times discusses the convenience of outpatient care for patients seeking efficient and flexible treatment options. Outpatient care refers to medical services that don't require an overnight stay in a hospital. This type of care allows you to receive the necessary treatment without disrupting your daily routine.
The article highlights two key advantages of outpatient care:
- Convenience: Outpatient care offers you the convenience of scheduling appointments that fit your busy schedule. You can receive treatment and return home on the same day, avoiding the hassle of staying overnight in a hospital.
- Cost-effective: Outpatient care is generally more cost-effective compared to inpatient care. You may not have to pay for hospital accommodation, which can significantly reduce your medical expenses.
Overall, outpatient care provides an efficient and flexible solution for patients seeking timely treatment while minimizing disruptions to their daily lives and financial burden.
Lower Healthcare Costs
Lowering healthcare costs is a top priority for many individuals looking to manage their medical expenses. One way to achieve this is by exploring different healthcare options that offer affordable alternatives without compromising quality. Here are some pros and cons of different healthcare options:
| Healthcare Option | Pros | Cons |
|---|---|---|
| Private Insurance | Wide range of coverage options | High premiums and out-of-pocket expenses |
| Medicaid | Low-income individuals can qualify | Limited provider network |
| Medicare | Coverage for elderly and disabled | Gaps in coverage and high deductibles |
| Health Savings Account (HSA) | Tax advantages and flexibility | Limited contribution limits and eligibility |
| Direct Primary Care | Affordable monthly fees | Limited specialist coverage |
Faster Recovery Time
To expedite your healing process, consider opting for outpatient treatment, as it can result in faster recovery time and greater convenience.
When you choose outpatient treatment, you have the advantage of returning home after your procedure, allowing you to recover in the comfort of your own surroundings. This can lead to reduced stress levels and a more positive mindset, both of which are crucial for a speedy recovery.
Additionally, outpatient treatment often involves less invasive procedures, which can minimize post-operative pain and discomfort.
Furthermore, outpatient facilities are designed to provide specialized care in a focused and efficient manner, ensuring that you receive the personalized attention you need.
Overall, by choosing outpatient treatment, you can significantly reduce your recovery time and enjoy the benefits of a quicker return to your daily activities.
Wide Range of Applications
You can explore the wide range of applications of interventional radiology to understand its versatility and effectiveness.
Interventional radiology is a medical specialty that uses minimally invasive procedures to diagnose and treat a variety of conditions.
One of the main advantages of interventional radiology is its ability to treat a wide range of diseases and conditions without the need for open surgery. For example, it can be used to treat blocked blood vessels, remove kidney stones, and even deliver targeted cancer treatments.
Additionally, interventional radiology can be used for diagnostic purposes, such as performing biopsies or imaging-guided procedures.
The versatility of interventional radiology makes it a valuable tool in modern medicine, allowing for precise and targeted treatments that can often be performed on an outpatient basis.
By offering less invasive alternatives to traditional surgery, interventional radiology can provide patients with faster recovery times, reduced pain, and fewer complications.
Overall, the wide range of applications of interventional radiology demonstrates its effectiveness in improving patient outcomes and quality of life.
Potential for Reduced Healthcare Costs
Interventional radiology has the potential to significantly reduce healthcare costs. By utilizing minimally invasive techniques, it can often replace more invasive surgical procedures, leading to shorter hospital stays and decreased post-operative care requirements. This not only reduces the financial burden on patients, but also on the healthcare system as a whole.
Here are some key points to consider regarding the potential for reduced healthcare costs through interventional radiology:
- Decreased hospitalization costs:
- Interventional radiology procedures are often performed on an outpatient basis, eliminating the need for costly hospital stays.
- Patients can return to their normal activities sooner, reducing lost productivity and minimizing the need for ongoing care.
- Lower complication rates:
- Interventional radiology procedures typically have lower complication rates compared to traditional surgical interventions.
- This can lead to fewer readmissions, reoperations, and associated healthcare costs.
Frequently Asked Questions
How Long Does It Typically Take to Perform an Interventional Radiology Procedure?
Typically, it takes about an hour to perform an interventional radiology procedure. This can vary depending on the complexity of the case and the specific procedure being done.
Are There Any Specific Conditions or Diseases That Cannot Be Treated With Interventional Radiology?
There are some conditions and diseases that cannot be treated with interventional radiology. However, it's important to discuss this within the context of the pros and cons of the procedure to fully understand its limitations.
Can Interventional Radiology Procedures Be Performed on Pediatric Patients?
Yes, interventional radiology procedures can be performed on pediatric patients. It's a safe and effective option for treating various conditions in children, offering minimally invasive techniques and faster recovery time.
Are There Any Potential Long-Term Side Effects of Interventional Radiology Procedures?
There may be potential long-term side effects of interventional radiology procedures. It is important to discuss these risks with your doctor and weigh them against the potential benefits before undergoing any procedure.
How Does Interventional Radiology Compare to Traditional Surgical Procedures in Terms of Success Rates?
Interventional radiology has a success rate of 90%, which is comparable to traditional surgical procedures. It offers less invasive options, shorter recovery time, and reduced risk of complications.